Since burning out I have recognised my need to check in with myself and measure my well-being and capacity to care regularly.
Colleagues who have worked with me laugh at my favourite classroom shout :
‘On a scale of 0 to 10 where 0 is sure and certain death and 10 is living your best life ever, where is your capacity to do this job right now?’
It’s dramatic and tongue in cheek but it does cause us to stop and think and share where we are at so we all pull together. That’s the joy of teams and as an unpaid carer I don’t always have a wider team to draw on, but checking in with myself and cutting myself respective slack seems healthy practice moving forwards.
I recognise the need to take this practice from my professional life and apply it to my Unpaid Carer role.
When I started to think about how to do this I realised that to be able to accurately scale my capacity I needed to identify what needs needed to be met for me to be able to fulfill my role. I had a look online at Maslow’s Heirarchy of Needs ( google it) and various associated well-being wheels and then, using a technical term: Jennie’d it. Here is the original drawing of what I arrived it, which doesn’t mean it’s a ‘one size, fits all carers’, but this one fits me and B on our wholehearted journey at this time .P.S. you should know we both have wild hair without TLC hence wild haired carer in middle!
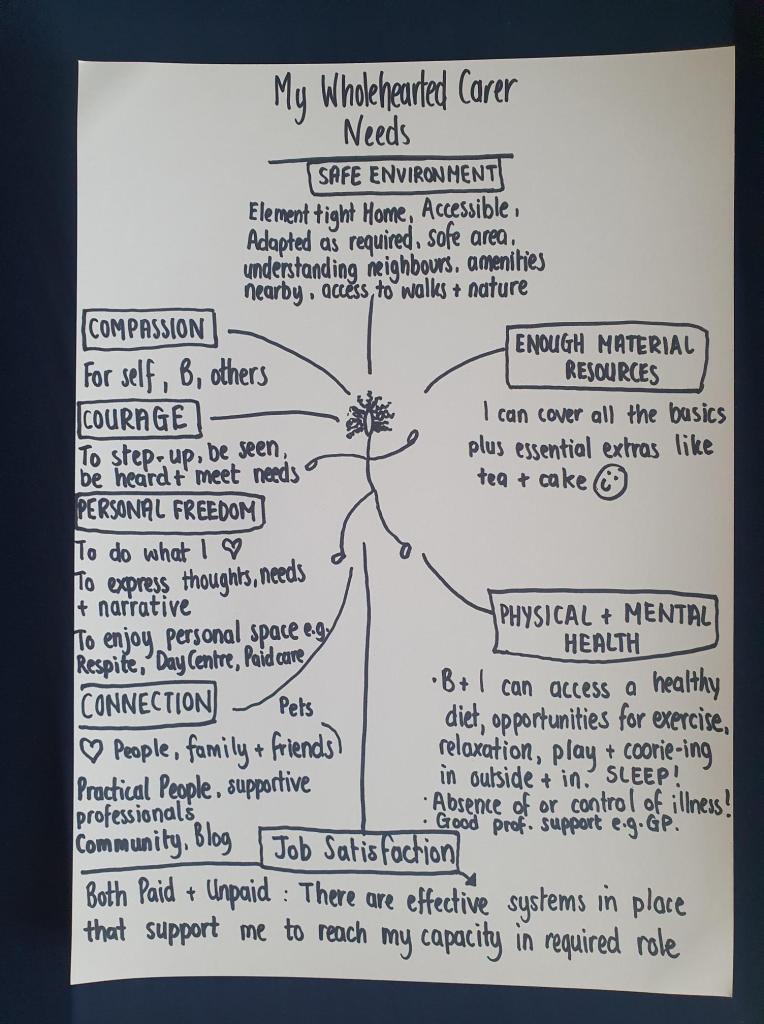
These are all the needs I need met to have full capacity to GO in my wholehearted caring role. I’m quite sure I’ve omitted things, but these are my gut responses. Obviously there will be times when some needs are better met than others, but I think it’s about looking at all the needs and thinking about it on balance. Here is my first draft capacity scale:
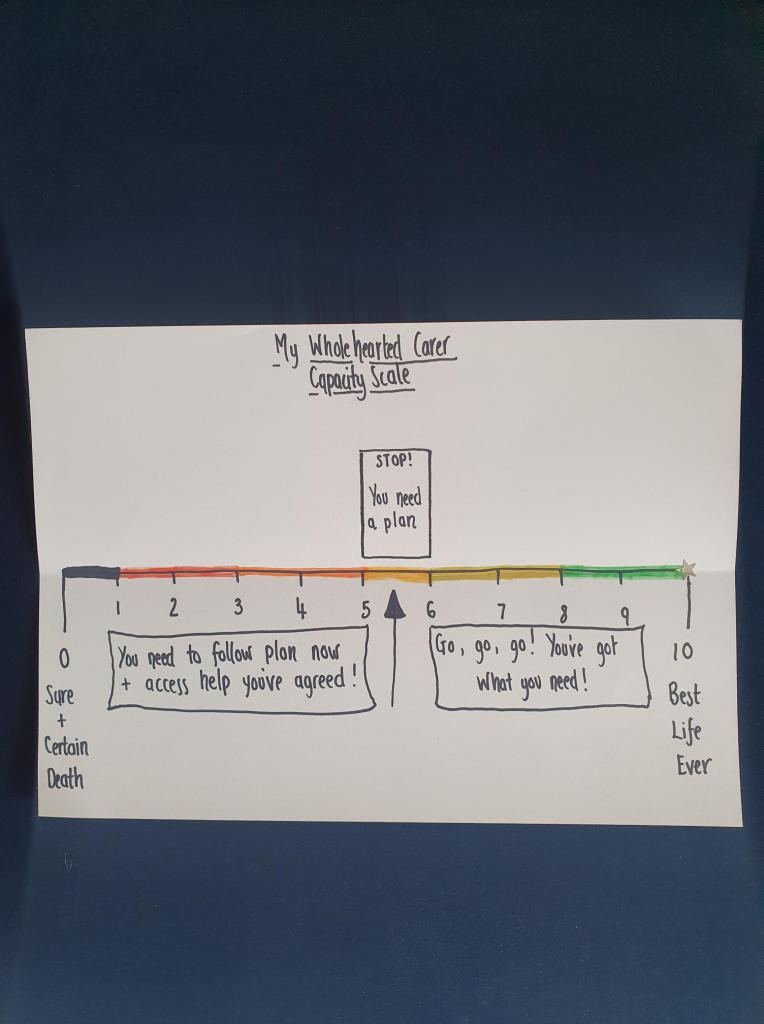
I found it helpful to think of the scale in increments of 10% so 0 is 0%, 5 is 50%, 10 is 100%. On balance, what percentage of my needs are being met? Today ( July 24th 2024) I find I am about a 7 maybe even an 8 as I’d say 70 to 80% of our identified needs are being met! I actually need to take a moment to celebrate this, because after many months scoring around 5 or below, this has been hard fought for. Our needs are being well met today! I have capacity to go! True it is the end of the month and my bank account could do with a boost, but on balance today is a good day and this is a golden moment! I realise there may be exceptions to the above rule, if I’ve got 80% on balance but close to 0% in one area e.g. physical and mental health then erm … that’s an issue that can’t wait and I might need to enact the plan ASAP – basically I need to trust my gut on what I need to action when!
I am generally a glass half full girl, but I know that I need to plan for when our needs aren’t so well met and my capacity slips. When I burnt out earlier this year, I had ignored some signs for months. I did know I was functioning below par, and I had gone to my GP for help with my stress levels, but her referral for Cognitive Behaviour Therapy took months and 6 months on the referral wasn’t through and I had taken no other action. In hindsight I’d hit 2 to 3 on the above scale. I want to try and prevent that happening again, so I developed this process and the following plan that I can put into practice as required:
My Wholehearted Carer’s Plan for 5 or below (or as required)
I, Jennie Webster, do solemnly swear 😉 that when I know myself to be at 5 or below on my capacity scale I need to:
STOP and take time to stand back and pay attention
LOOK at my identified needs and work out what needs are challenged. Often I know needs knock on to each other so my mental health needs may not be being met because B is falling a lot and I’m feeling anxious and overwhelmed. I need to remember to take a challenge at a time to avoid overwhelm.
APPLY the adapted serenity prayer philosophy to each challenge:
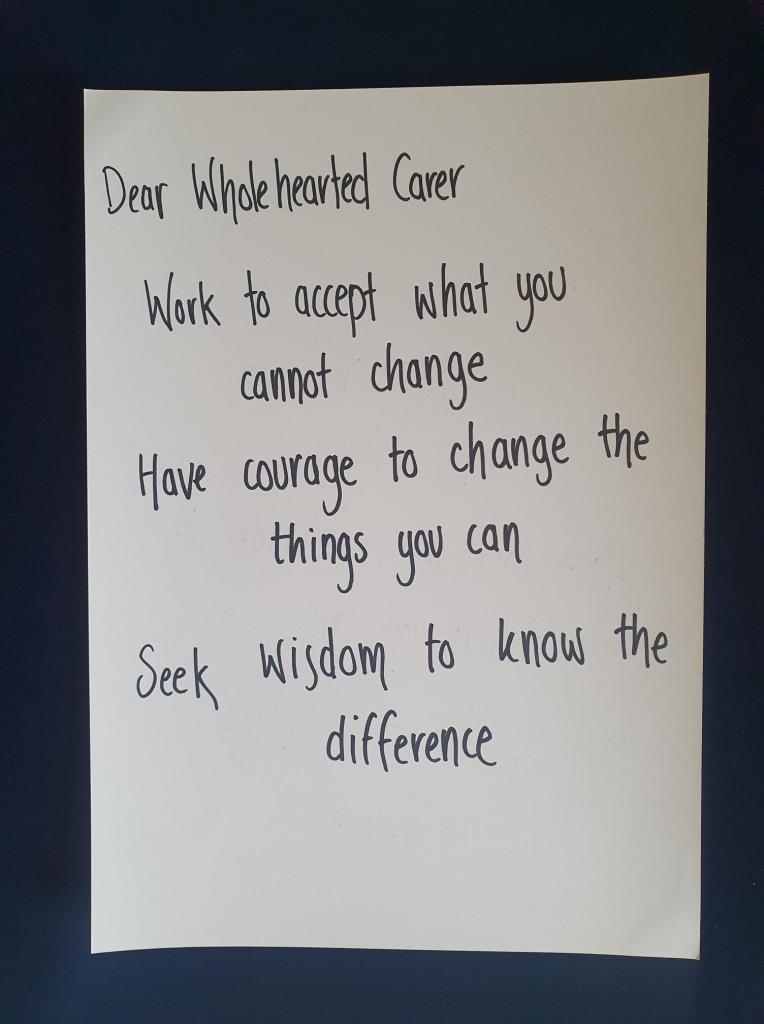
ASK can I change this challenge? Sometimes I find this may be a yes and no situation.
ANSWER Yes! Plan what steps I need to take to change it , with whom ( heart and/or practical people?) e.g. If B is falling more I need to work out any factors that are increasing falls, then contact the physio ( practical person) and share with her and ask her out to the house to assess fall risks and make any adaptations or referrals to prevent further falls.
ANSWER No! Plan what steps I need to foster acceptance about what cannot be changed, and with whom. e.g. B’s condition is degenerating, she is falling more often, this is emotionally painful and that pain is decreasing my capacity. To work towards acceptance I need to share with my close friends and family (heart people) and maybe even a mental health professional if this is bordering on complex grief/ depression (practical people). I may also need a good night out with friends, dancing and wine!
REMEMBER I am NOT an island and it is part of my self care to reach out to others.
Note on Heart and Practical People and Community:
This is the picture I drew when I was figuring out who I needed to surround myself with. I realise now that there could be confusion around the term ‘capacity and willingness to step in to care with and for me’. When I wrote this I intended the meaning to be that they would step in to care for B in my place, but I realise it could be read as care for me as an individual separate from B. I wondered if I should edit it before posting, but actually my Heart People do care for B and I as individuals, so I’m sticking with my original scribblings. The Heart People are my core, surrounded by the Practical People, I need both. Community and Society are in the big, blue beyond.
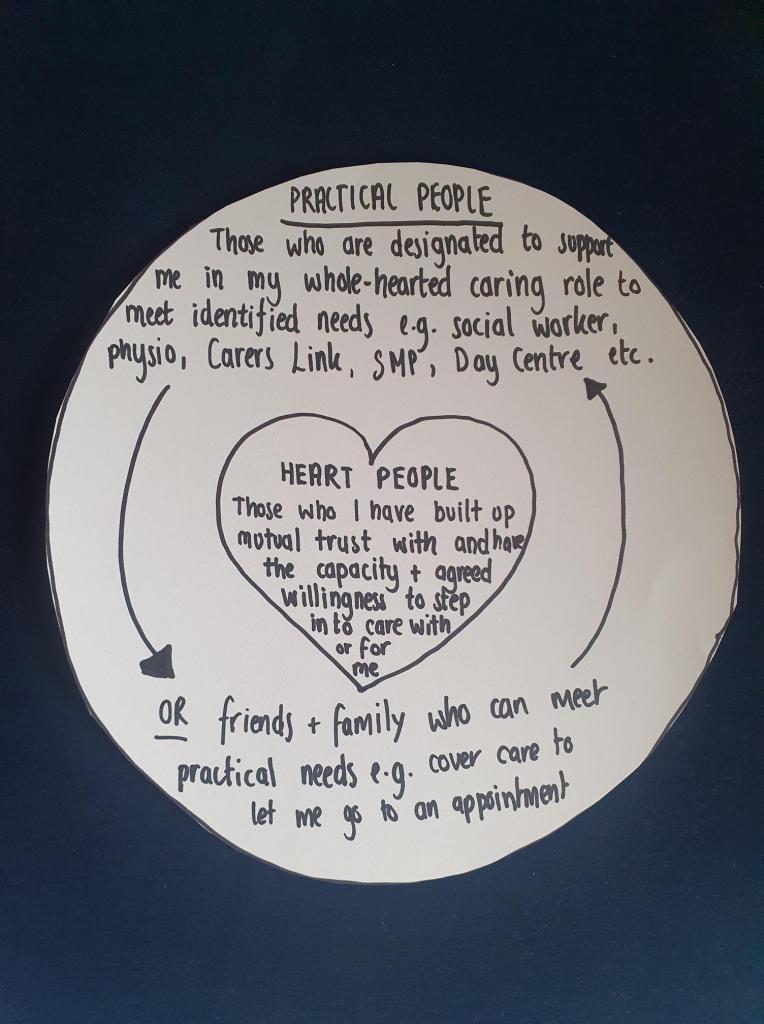
I know who my Heart People are. They are a small group of family and friends where our love is mutual, reciprocated and strong. Heart People are my deep dive people, who can provide support including but far beyond the practical. They are the people who sit in empathy not judgement or pity and value my vulnerabilities as strength. They build me up, don’t break me down. They are the people who let me ramble and listen, even as I don’t have the words to articulate any mental sticking points. Heart people are the people who have shared hard times with me and the sharing has strengthened not strained our bond. They are the tried and tested loved ones, but more than that they are the tried and tested loved ones who have capacity and willingness to step into my wholehearted caring role if I need them to.They know I may need this of them and have agreed to it. We have had this chat.
Practical People are the people who can meet practical needs, they might be a heart person too, like a family member who can cover care to let me go out or they might be part of the established system of support e.g. social worker, GP, Physio, Local Carer’s Association, B’s personal assistant etc.
And then there’s the Community that may grow from sharing this blog and I’m not quite sure where that will go? I suspect if a community forms it may have potential to meet both heart and practical needs for all involved. It’ll be exciting to see what blossoms from this seed.
A closing thought on how asking for help links with Empowerment, Courage and Vulnerability
I know previously, that I really struggled to reach out to others. I saw it as my sole responsibility to meet B’s needs. I saw it as weakness to ask for help and found being vulnerable painful, and yet I wanted and want to be empowered. There is this undeniable relationship between empowerment, community and wider society. I can’t think of one empowered person or movement that has operated in isolation without community or society! I suppose the critic could argue that is due to their isolation, but I also think there’s something about empowerment that demands sharing and community. We can only have power and rights in relation to other’s.
If I seek to be an empowered carer then I need to reach out beyond B and I. It is not my individual capacity to care dropping below 5 that threatens my empowerment as a wholehearted carer, it is my inability or refusal to reach out to my wider community for help that ultimately could fail B. I have the right to be supported, but I need to be able to ask for help. My vulnerability in doing so is not weak, it’s courage. I’m paraphrasing, but Brene Brown defines vulnerability as uncertainty, risk and emotional exposure and writes of delivering a talk to individuals from the armed forces and inviting them to, ‘Name one act of courage that doesn’t involve uncertainty, risk, and emotional exposure’? I can’t think of one, and according to Brown, neither could they. Courage and vulnerability are inextricably linked, the root of the word ‘courage’ is the latin ‘cor’ which means heart. Wholehearted carer’s are courageous in their vulnerability not in spite of it. It takes courage to be vulnerable and to ask for help, and it takes belief that we are inherently worthy of that help. I believe that B and I are worthy members of society who have a right to call on support from that society.
‘A true measure of any society can be found in how it treats its most vulnerable members’ Mahatma Gandhi
NOTE ON CAPACITY SCALE 1: I’d add that if I am at 2 or below I’m probably not in the head space to follow my plan and in that instance it’d be good if my heart people knew my plan in advance so they can support me back to working capacity ;-).
NOTE 2: My local Carer’s Support Agency ‘Carer’s Link’ offer a service to draft a Carer’s Emergency Plan. I have had this done, although in looking it out I realise I need to get it updated. This is kept on file with ‘Carer’s Link’ and contains emergency contact details ( heart people ;-)); B’s medical info; details of B’s typical day/week and key info ( B’s likes/dislikes). This process is worth doing for peace of mind should I ever be completely incapacitated and can complement the above process rather than replace it, the above process is perhaps the ‘heart process’ whereas a ‘Carer’s Emergency Plan’ is the ‘practical process’ though there is always overlap between the two.

Leave a comment